HOME > SERVICES > EVALUATION AND MANAGEMENT OF VASCULAR DISEASE > Varicose Veins and Venous Insufficiency >
Varicose Veins and Venous Insufficiency
Varicose Veins and Venous Insufficiency
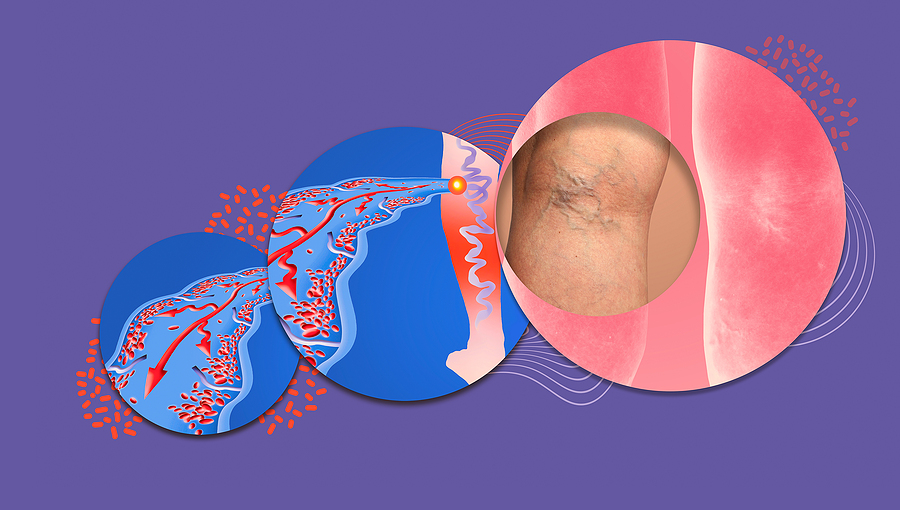
The veins in your legs carry blood back to your heart. They have one-way valves that keep blood from flowing backward. If you have chronic venous insufficiency (CVI), the valves don’t work like they should and some of the blood may go back down into your legs. That causes blood to pool or collect in the veins.
Over time, CVI can cause pain, swelling, and skin changes in your legs. It may also lead to open sores called ulcers on your legs.
You may notice these in your legs:
- Swelling or heaviness, especially in the lower leg and ankle
- Pain
- Itchiness
- Varicose veins (twisted, enlarged veins close to the surface of the skin)
- Skin that looks like leather
Without treatment, the pressure and swelling will burst the tiny blood vessels in your legs called capillaries. That could turn your skin reddish-brown, especially near the ankles. This can lead to swelling and ulcers. These ulcers are tough to heal. They are also more likely to get infected, which can cause more problems.
If you have any of the symptoms of CVI, talk to your doctor. The sooner you treat it, the less likely you’ll get ulcers.
A blood clot in a deep vein in your leg (called deep vein thrombosis) can damage a valve. If you don’t exercise, that can cause CVI, too. So can sitting or standing for long stretches of time. That raises pressure in your veins and may weaken the valves.
Women are more likely than men to get CVI. Your chances also might be higher if you are:
- Obese
- Over age 50
- Pregnant or have been pregnant more than once
- From a family with a history of CVI
- Someone with history of blood clots
- A smoker
Your doctor will take your medical history. They then will check the blood flow in your legs with a test called a vascular or duplex ultrasound. Your doctor will place a small device on your skin over the vein. Using sound waves, they can see the blood vessel and check how quickly and in what direction the blood flows.
Sometimes, you may need X-rays or specific scans to check for other causes of your leg swelling.
The main goal is to stop swelling and prevent leg ulcers. Your doctor may suggest a combination of treatments based on your age, symptoms, and other things. Some options to help manage CVI include:
Lifestyle Changes
You can help blood flow better in your leg veins. Steps include:
Compression stockings. These elastic socks put pressure on your legs to help blood move. They come in different tightnesses, lengths, and styles. Your doctor can suggest which might work best for you.
Movement. Try not to sit or stand for a long time. If you have to sit for a while, stretch or wiggle your legs, feet, and ankles often to help your blood flow. If you stand a lot, take breaks to sit and put your feet up. This helps lower pressure in your leg veins.
Exercise. Working out helps pump your blood, too. Walking is a good, simple way to make your legs stronger and boost blood flow.
Medications
Your doctor may prescribe an antibiotic to treat infections or leg ulcers. Sometimes, they’ll give you medicine to help prevent blood clots.
Medical Procedures
If your CVI is further along, you may need a nonsurgical treatment.
Sclerotherapy. Your doctor will inject a solution into the problem vein. It scars the vein, forcing blood to flow through healthier veins. Over time, your body absorbs the scarred vein.
Endovenous thermal ablation. This newer method uses high-frequency radio waves or a laser to heat and close the problem vein.
Surgery
Fewer than 1 in 10 people need surgery for CVI.
Here are your options:
Ligation. The vein is cut and tied off so blood can’t flow through. Your doctor may also remove a vein that is very damaged. You usually will go home on the same day.
Microincision/ambulatory phlebectomy. This technique uses much smaller incisions, punctures and small hooks to remove damaged veins.
Vein repair. Your doctor fixes the vein or the valves. This can be done through an open cut on your leg or through a smaller opening by using a long, hollow catheter or tube.
Vein transplant. Your doctor replaces the problem vein with a healthy one from somewhere else in your body.
Vein bypass. This is done on veins in the upper thigh and only in the most severe cases. Your doctor takes part of a healthy vein from another part of your body. They’ll use that to reroute blood around the affected vein. You’ll usually stay in the hospital for 2-5 days.

