HOME > SERVICES > EVALUATION AND MANAGEMENT OF VASCULAR DISEASE > Abdominal Aortic Aneurysm >
Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm
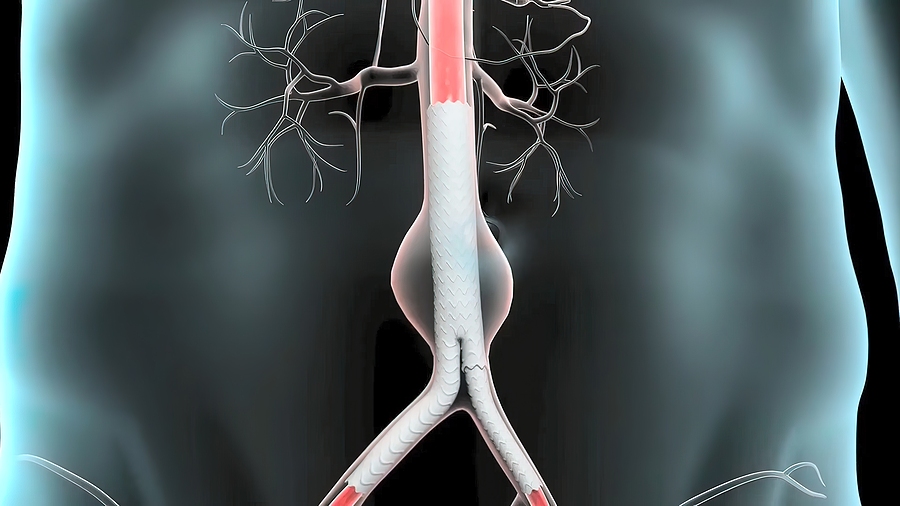
An abdominal aortic aneurysm is an enlarged area in the lower part of the major vessel that supplies blood to the body (aorta). The aorta runs from the heart through the center of the chest and abdomen.
The aorta is the largest blood vessel in the body, so a ruptured abdominal aortic aneurysm can cause life-threatening bleeding.
Depending on the size of the aneurysm and how fast it’s growing, treatment varies from watchful waiting to emergency surgery.
Abdominal aortic aneurysms often grow slowly without noticeable symptoms, making them difficult to detect. Some aneurysms never rupture. Many start small and stay small. Others grow larger over time, sometimes quickly.
If you have an enlarging abdominal aortic aneurysm, you might notice:
- Deep, constant pain in the belly area or side of the belly (abdomen)
- Back pain
- A pulse near the bellybutton
If you have pain, especially if pain is sudden and severe, seek immediate medical help.
Aneurysms can develop anywhere along the aorta, but most aortic aneurysms occur in the part of the aorta that’s in the belly area (abdomen). Several things can play a role in the development of an abdominal aortic aneurysm, including:
- Hardening of the arteries (atherosclerosis). Atherosclerosis occurs when fat and other substances build up on the lining of a blood vessel.
- High blood pressure. High blood pressure can damage and weaken the aorta’s walls.
- Blood vessel diseases. These are diseases that cause blood vessels to become inflamed.
- Infection in the aorta. Rarely, a bacterial or fungal infection might cause an abdominal aortic aneurysms.
- Trauma. For example, being injured in a car accident can cause an abdominal aortic aneurysms.
Abdominal aortic aneurysm risk factors include:
- Tobacco use. Smoking is the strongest risk factor for aortic aneurysms. Smoking can weaken the walls of the aorta, increasing the risk of aortic aneurysm and aneurysm rupture. The longer and more you smoke or chew tobacco, the greater the chances of developing an aortic aneurysm. Doctors recommend a one-time abdominal ultrasound to screen for an abdominal aortic aneurysm in men ages 65 to 75 who are current or former cigarette smokers.
- Age. Abdominal aortic aneurysms occur most often in people age 65 and older.
- Being male. Men develop abdominal aortic aneurysms much more often than women do.
- Being white. People who are white are at higher risk of abdominal aortic aneurysms.
- Family history. Having a family history of abdominal aortic aneurysms increases the risk of having the condition.
- Other aneurysms. Having an aneurysm in another large blood vessel, such as the artery behind the knee or the aorta in the chest (thoracic aortic aneurysm), might increase the risk of an abdominal aortic aneurysm.
If you’re at risk of an aortic aneurysm, your doctor might recommend other measures, such as medications to lower your blood pressure and relieve stress on weakened arteries.
Tears in one or more of the layers of the wall of the aorta (aortic dissection) or a ruptured aneurysm are the main complications. A rupture can cause life-threatening internal bleeding. In general, the larger the aneurysm and the faster it grows, the greater the risk of rupture.
Signs and symptoms that an aortic aneurysm has ruptured can include:
- Sudden, intense and persistent abdominal or back pain, which can be described as a tearing sensation
- Low blood pressure
- Fast pulse
Aortic aneurysms also increase the risk of developing blood clots in the area. If a blood clot breaks loose from the inside wall of an aneurysm and blocks a blood vessel elsewhere in your body, it can cause pain or block blood flow to the legs, toes, kidneys or abdominal organs.
To prevent an aortic aneurysm or keep an aortic aneurysm from worsening, do the following:
- Don’t smoke or use tobacco products. Quit smoking or chewing tobacco and avoid secondhand smoke. If you need help quitting, talk to your doctor about medications and therapies that may help.
- Eat a healthy diet. Focus on eating a variety of fruits and vegetables, whole grains, poultry, fish, and low-fat dairy products. Avoid saturated and trans fats and limit salt.
- Keep your blood pressure and cholesterol under control. If your doctor has prescribed medications, take them as instructed.
- Get regular exercise. Try to get at least 150 minutes a week of moderate aerobic activity. If you haven’t been active, start slowly and build up. Talk to your doctor about what kinds of activities are right for you.

